Assessment and diagnosis of recent onset chest pain or discomfort of suspected cardiac origin
For pain that is suspected to be cardiac, there are two separate diagnostic pathways considered by NICE (1)
- the first is for people with acute chest pain and a suspected acute coronary syndrome
- the second is for people with intermittent stable chest pain in whom stable angina is suspected
Presentation with acute chest pain
- a resting 12-lead electrocardiogram (ECG) should be undertaken as soon as possible. When people are referred, send the results to hospital before they arrive if possible. Recording and sending the ECG should not delay transfer to hospital
- do not exclude an acute coronary syndrome (ACS) when people have a normal resting 12-lead ECG
- oxygen should not routinely administered, but monitor oxygen saturation using pulse oximetry as soon as possible, ideally before hospital admission. Supplemental oxygen should only be offered to:
- people with oxygen saturation (SpO2) of less than 94% who are not at risk of hypercapnic respiratory failure, aiming for SpO2 of 94-98%
- people with chronic obstructive pulmonary disease who are at risk of hypercapnic respiratory failure, to achieve a target SpO2 of 88-92% until blood gas analysis is available
- symptoms of an ACS should not be assessed differently in ethnic groups. There are no major differences in symptoms of an ACS among different ethnic groups
Presentation with stable chest pain
- stable angina should be diagnosed based on one of the following:
- clinical assessment alone or
- clinical assessment plus diagnostic testing (that is, anatomical testing for obstructive coronary artery disease [CAD] and/or functional testing for myocardial ischaemia)
- if people have features of typical angina based on clinical assessment and their estimated likelihood of CAD is greater than 90% (see tables), further diagnostic investigation is unnecessary. Manage as angina
Table 1: Non-anginal chest pain - % likelihood of CAD
Men | Men | Women | Women | |
Age (years) | Lo | Hi | Lo | Hi |
35 | 3% | 35% | 1% | 19% |
45 | 9% | 47% | 2% | 22% |
55 | 23% | 59% | 4% | 45% |
65 | 49% | 69% | 9% | 49% |
Table 1 represents people with symptoms of non-anginal chest pain, who would not be investigated for stable angina routinely
Table 2: Atypical anginal pain - % likelihood of CAD
Men | Men | Women | Women | |
Age (years) | Lo | Hi | Lo | Hi |
35 | 8% | 59% | 2% | 39% |
45 | 21% | 70% | 5% | 43% |
55 | 45% | 79% | 10% | 47% |
65 | 71% | 86% | 20% | 51% |
Table 3: Typical angina - % likelihood of CAD
Men | Men | Women | Women | |
Age (years) | Lo | Hi | Lo | Hi |
35 | 30% | 88% | 10% | 78% |
45 | 51% | 92% | 20% | 79% |
55 | 80% | 95% | 38% | 82% |
65 | 93% | 97% | 56% | 84% |
- for men older than 70 with atypical or typical symptoms, assume an estimate > 90%.
- For women older than 70, assume an estimate of 61-90% EXCEPT women at high risk AND with typical symptoms where a risk of > 90% should be assumed
- Values are per cent of people at each mid-decade age with significant coronary artery disease (CAD)
- Hi = High risk = diabetes, smoking and hyperlipidaemia (total cholesterol > 6.47 mmol/litre)
- Lo = Low risk = none of these three
- Note:
- These results are likely to overestimate CAD in primary care populations. If there are resting ECG ST-T changes or Q waves, the likelihood of CAD is higher in each cell of the table.
Unless clinical suspicion is raised based on other aspects of the history and risk factors, exclude a diagnosis of stable angina if the pain is non-anginal
Other features which make a diagnosis of stable angina unlikely are when the chest pain is:
- continuous or very prolonged and/or
- unrelated to activity and/or
- brought on by breathing in and/or
- associated with symptoms such as dizziness, palpitations, tingling or difficulty swallowing. Consider causes of chest pain other than angina (such as gastrointestinal or musculoskeletal pain).
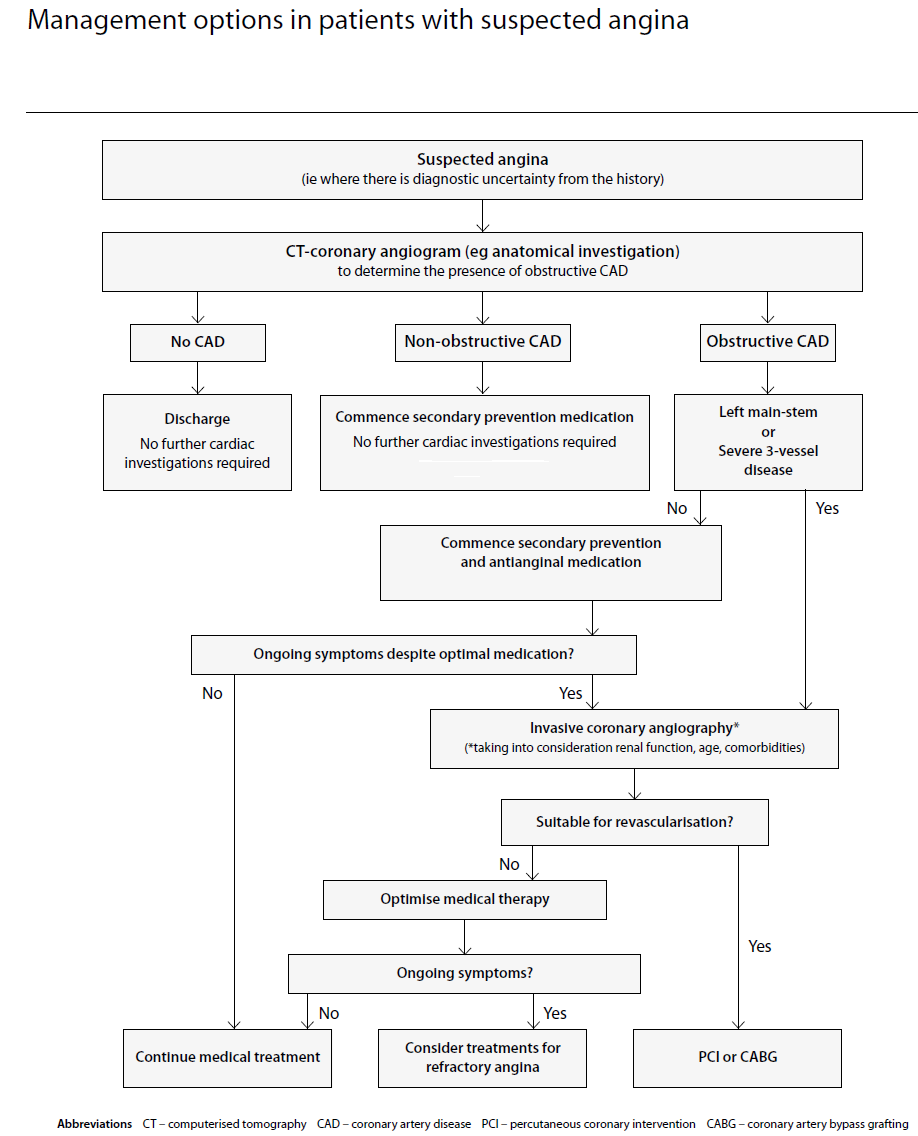
- SIGN consider options in investigation and management in context of whether patient has "suspected angina" (2):
Reference:
- NICE. Recent-onset chest pain of suspected cardiac origin: assessment and diagnosis. Clinical guideline [CG95]Published: 24 March 2010 Last updated: 30 November 2016
- SIGN (April 2018). Management of Stable Angina
Related pages
- Chest pain
- In patients without known coronary artery disease in whom the diagnosis of stable angina cannot be excluded
- Initial assessment and referral to hospital of possible acute chest pain of cardiac origin
- Assessment of stable chest pain of suspected cardiac origin
- Factors that make a diagnosis of stable angina unlikely
Create an account to add page annotations
Add information to this page that would be handy to have on hand during a consultation, such as a web address or phone number. This information will always be displayed when you visit this page