Pemphigoid gestationis
Pemphigoid gestationis is a severe bullous eruption that occurs in 1 in 60,000 pregnancies.
It is unusual for a primigravid women to be affected. In affected women the skin lesions become progressively more severe during successive pregnancies.
- self-limited autoimmune bullous disorder that presents mainly in late pregnancy or the immediate postpartum period but can appear in any of the three trimesters
- beyond pregnancy it can also very rarely occur in association with trophoblastic tumors (choriocarcinoma, hydatidiform mole)
- also an increased risk to develop other autoimmune diseases, in particular Grave's disease
- pemphigoid gestationis tends to recur in subsequent pregnancies, with usually earlier onset and increasing severity. Only very rarely (5%) a pregnancy may be passed over
Pemphigoid gestationis presents with intense pruritus that occasionally may precede the manifestation of skin lesions
- initially, erythematous urticarial papules and plaques typically develop on the abdomen
- in this so-called pre-bullous stage, differentiation between pemphigoid gestationis and polymorphic eruption of pregnancy is almost impossible, both clinically and histopathologically
- occurs during the second and third trimesters of pregnancy
- initial sites include the periumbilical area, around the mouth, palms and soles
- later lesions may become widespread
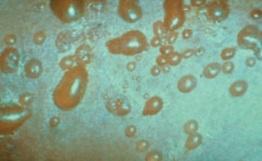
- after about 4 weeks bullous lesions appear bullous lesions resolve about 4 weeks post-partum
Risk for fetus
- increase in prematurity and small-for-date babies
- neonatal pemphigus is a rare complication of pregnancy in pemphigus patients
Treatment
- seek expert advice
- depends on the stage and severity of the disease and aims to control pruritus and to prevent blister formation
- in cases of mild pre-blistering pemphigoid, topical corticosteroids with or without oral antihistamines may be sufficient
- all other cases require systemic corticosteroids
- severe cases may benefit from immunoapheresis
- after delivery, if necessary, other immunosuppressive treatment may be used
Reference:
- 1) Ambros-Rudolph CM. Dermatoses of pregnancy - clues to diagnosis, fetal risk and therapy. Ann Dermatol. 2011 Aug;23(3):265-75.
- 2) Daneshpazhooh M et al. Pemphigus and pregnancy: a 23-year experience.Indian J Dermatol Venereol Leprol. 2011 Jul-Aug;77(4):534.
Related pages
Create an account to add page annotations
Add information to this page that would be handy to have on hand during a consultation, such as a web address or phone number. This information will always be displayed when you visit this page