Assessment of unscheduled bleeding if taking hormonal contraception
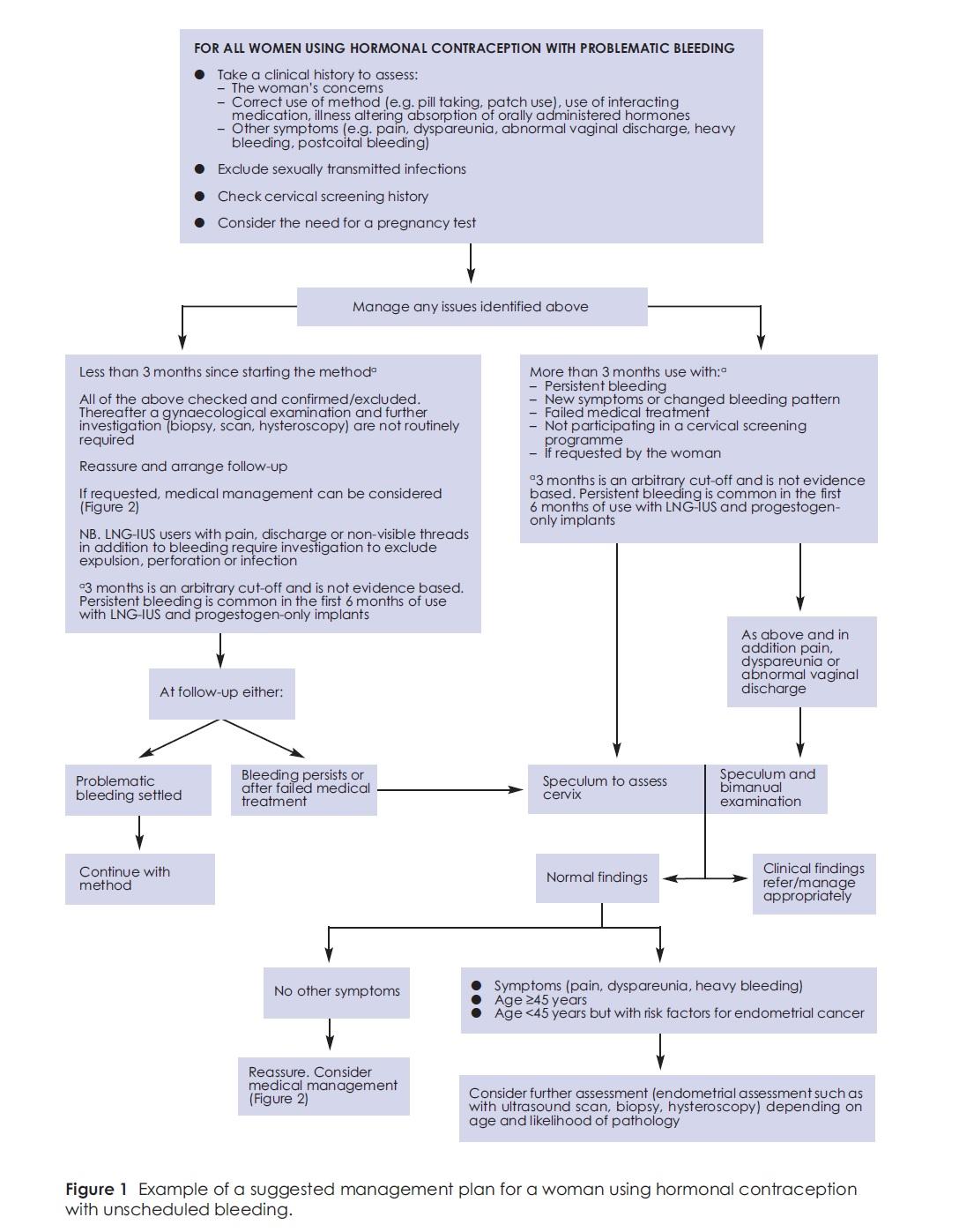
The management of women with unscheduled bleeding in the initial months (i.e. 3-6 months) after starting a new method of hormonal contraception may differ from that of women who continue to have unscheduled bleeding in the longer term or who present with a change in bleeding pattern
A clinical history should highlight possible underlying causes (an example being Chlamydia trachomatis) and provide a guide to the most appropriate examination, investigation and treatment options required.
Reassuringly in community populations, endometrial cancer is very rare in women of reproductive age who are using hormonal contraception or who do not have risk factors for endometrial cancer (such as obesity, polycystic ovarian syndrome, tamoxifen use or unopposed estrogen therapy). Cervical cancer is also rare in this population, especially in women who comply with National Cervical Screening Programmes.
Points to cover in the clinical history from a woman using hormonal contraception who presents with unscheduled bleeding Clinical history taking should include an assessment of the woman's:
a Progestogen-only methods are more likely to present with unscheduled bleeding than combined hormonal methods, and bleeding with progestogen-only pills is less likely to settle than bleeding with the progestogen-only injectable. b For example, missed pills. c A woman presenting with abnormal bleeding who is participating in a National Cervical Screening Programme does not require a cervical screen unless one is due. |
All women using hormonal contraception who have unscheduled bleeding should be assessed to identify the risk of sexually transmitted infections (STIs)
- chlamydia trachomatis is the most common bacterial STI in the UK and although up to 80% of women with C. trachomatis are asymptomatic abnormal bleeding may be a presenting symptom
- risk factors for STIs include age <25 years, or a new sexual partner, or more than one partner in the last year
- if deemed at risk for an STI, C. trachomatis should be excluded as a minimum
- a single vaginal swab can be sent for combined C. trachomatis and Neisseria gonorrhoea testing by nucleic acid amplification testing. Vaginal swabs can be self-taken if preferred. Urine testing is no longer recommended for STI screening in women.
A cervical screening test is not a diagnostic test of cancer. The cervical screening history should be checked to ensure that women are participating in a National Cervical Screening Programme. This may have been checked when hormonal contraception was initiated but should be reviewed if a woman presents with unscheduled bleeding. A cervical screen can be taken if due or overdue. No evidence was identified to support cervical screening if not due.
A pregnancy test should be undertaken in sexually active women with problematic bleeding using hormonal contraception. However, no evidence was identified which suggested that problematic bleeding in a woman who has been using hormonal methods consistently and correctly is associated with an increased risk of pregnancy
When may examination NOT be required?
- unscheduled bleeding in the first 3 months after starting a new hormonal contraceptive method is common.
- genital examination is not required if after taking a clinical history there are no risk factors for STIs, no concurrent symptoms suggestive of underlying causes, and the woman is participating in a National Cervical Screening Programme. Some women may be happy to continue with the method after this initial assessment but follow-up should be planned as bleeding may persist, other symptoms or concerns
When is examination required?
- providing there has been consistent and correct use of hormonal contraception, examination is warranted to visualise the cervix by speculum examination :
- For persistent bleeding beyond the first 3 months use
- For new symptoms or a change in bleeding after at least 3 months use of a method
- If the woman has not participated in a National Cervical Screening Programme
- If requested by the woman
- After a failed trial of the limited medical management available
- If there are other symptoms such as pain, dyspareunia or postcoital bleeding (NB. These symptoms would also warrant bimanual examination.)
Notes:
- the 3-month cut-off is given here as a guide only as some methods, in particular the IUS or progestogen only implant, may commonly cause bleeding after the first 3 months of use
- visualisation of the cervix can identify cervical conditions (such as polyps or ectopy), which may warrant referral for appropriate management. Most cases of cervical cancer are identified by screening. However, visualisation of the cervix may identify the very occasional case of cervical cancer that can present with abnormal vaginal bleeding. Referral for gynaecological examination and an urgent referral to colposcopy is required if cancer is suspected on examination
- visualisation of the cervix can identify cervical conditions (such as polyps or ectopy), which may warrant referral for appropriate management. Most cases of cervical cancer are identified by screening. However, visualisation of the cervix may identify the very occasional case of cervical cancer that can present with abnormal vaginal bleeding. Referral for gynaecological examination and an urgent referral to colposcopy is required if cancer is suspected on examination
- guidance from the National Institute for Health and Clinical Excellence (NICE) on the management of women with heavy menstrual bleeding recommends a speculum and bimanual examination if there are additional symptoms (such as intermenstrual or post-coital bleeding, pelvic pain or pressure symptoms suggestive of a structural or histological abnormality). This advice about examinations is appropriate for women with unscheduled bleeding using hormonal contraception
- providing there has been consistent and correct use of hormonal contraception, a speculum examination should be performed for women using hormonal contraception with unscheduled bleeding if they have: persistent bleeding or a change in bleeding after at least 3 months use; failed medical treatment; if they have not participated in a National Cervical Screening Programme
- providing there has been consistent and correct use of hormonal contraception in addition to a speculum examination, a bimanual examination should be performed for women using hormonal contraception with unscheduled bleeding if they have other symptoms (such as pain, dyspareunia or heavy bleeding)
- in general, an endometrial biopsy should be considered in women aged > =45 years (or in women aged <45 years with risk factors for endometrial cancer (e.g. obesity or polycystic ovarian syndrome) who have persistent problematic bleeding after the first 3 months of starting a method or who present with a change in bleeding pattern
- the role of uterine polyps, fibroids or ovarian cysts as a cause of unscheduled bleeding is limited. Nevertheless, for all women using hormonal contraception with unscheduled bleeding, if such a structural abnormality is suspected a transvaginal ultrasound scan and/or hysteroscopy may be indicated
Reference:
- FSRH (2015). Problematic bleeding with hormonal contraception.
Related pages
Create an account to add page annotations
Add information to this page that would be handy to have on hand during a consultation, such as a web address or phone number. This information will always be displayed when you visit this page