Prognosis of ALL
The following factors are associated with prognosis in ALL patients:
- age at diagnosis is considered to be a strong prognostic factor. According to a study carried out at children’s Research Hospital with 847 children with ALL:
- children between the age 1 to 9 had a better outcome than infants or adolescents. The 5 year event free survival estimates were (1)
- for children aged 1-9 - 88%
- adolescents aged 10–15 years - 73%
- older than 15 years - 69%
- babies younger than 12 months - 44%
- prognosis was poor especially for babies younger than 6 months
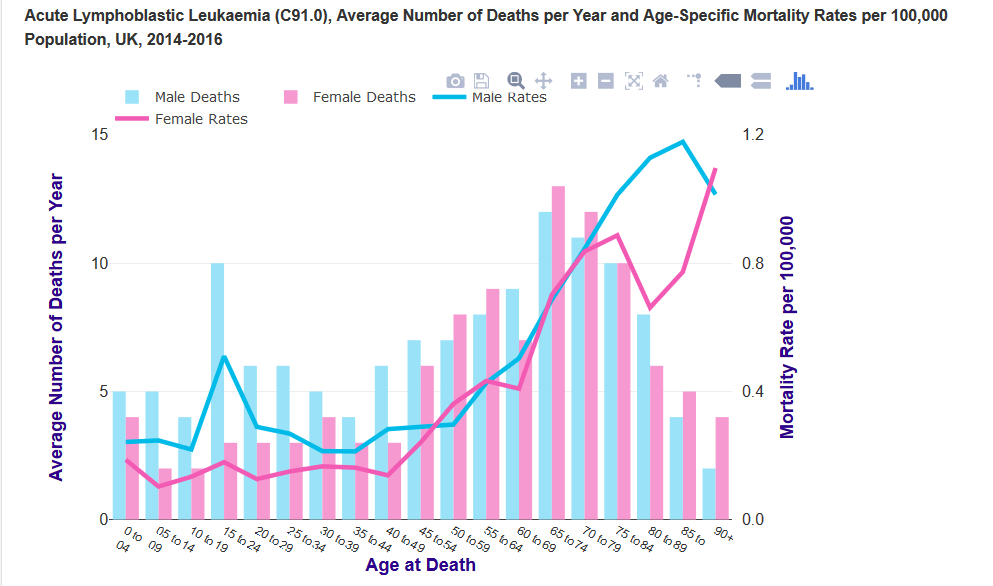
- age-specific mortality rates rise steadily from birth and more steeply from around age 45-49. The highest rates are in the 85 to 89 age group for males and the 90+ age group for females (2)
- increased leukocyte count presents with poor prognostic outcome.
- this is especially true in patients with B-cell precursor disease
- in T cell ALL, a count of more than 100x109/L is associated with an increased risk of relapse in the CNS
- high risk of early complications are seen in patients with extreme hyperleucocytosis (>400x109/L) e.g - CNS haemorrhage and pulmonary and neurological events due to leucostasis (1)
- chromosomal abnormality
- poorer outcome is also associated with Philadelphia chromosome, t(4;11) with MLL-AF4 fusion, and hypodiploidy (<44 chromosomes per leukaemic cell)
- favourable prognosis was seen in patients with hyperdiploidy (>50 chromosomes), TEL-AML1fusion, and trisomy 4, 10, and 17
Children respond well to treatment:
- 95% achieve complete remission
- 50-60% of whom are cured with postremission chemotherapy
Fewer advances have been achieved in adults:
- 80% achieve complete remission
- about 35% achieve long-term disease-free survival
The poorer response seen in adults may reflect undertreatment because of the increased risk of drug toxicity.
Reference:
Related pages
Create an account to add page annotations
Add information to this page that would be handy to have on hand during a consultation, such as a web address or phone number. This information will always be displayed when you visit this page